On that life-changing morning — January 28, 2020, a Tuesday — Springsteen was at her home with her boyfriend, Jeremiah Axtell. An attorney and newly elected member of Lakewood’s city council, Springsteen was known for pushing growth caps and challenging well-connected development interests. She was also embroiled in a long-running dispute with the operators of a memory-care center across the street from her house over several matters, from alleged elder abuse to improper disposal of human waste.
That morning, Axtell had a heated conversation with an employee of the center about a soiled adult diaper in the street. Someone from the center called 911, claiming that Axtell had a knife. When Lakewood police officers arrived, Axtell stepped into the street to greet them, removing his jacket and lifting his shirt to demonstrate that he was unarmed. That didn’t deter one officer from pointing her taser at him. Fearful of what might happen next, Springsteen began recording the incident on her phone.
Axtell, who would later admit to having a couple of drinks that morning, sat down in Springsteen’s driveway. He was soon surrounded by police and handcuffed. The cell-phone video shows him speaking calmly to the officers, promising to cooperate, then yelping with pain when they pull on his arms or the handcuffs. He showers them with curses and expresses frustration that he’s the one being arrested. “I didn’t do nothing wrong,” he fumes.
The frustration spikes after an emergency medical team from West Metro Fire Rescue arrives on the scene. A paramedic’s rote questions about whether he is on drugs and his grasp on reality draws an emphatic response. “Talk to me like a real person,” Axtell insists. “Goddamn it, you’re not even listening to me.”
But however agitated Axtell might have been, he offered no physical resistance to the responders as the encounter dragged on. The video shows him standing up and walking placidly under escort toward a patrol car, promising to comply “100 percent.”
That scene is in stark contradiction to the paramedic’s version. According to his report, Axtell “became combative and verbally aggressive” and yelled “random things that didn’t make sense” between fits of laughter. Although the patient was handcuffed and “oriented to person, place, time, and event,” the paramedic deemed him “uncontrollable…It was determined patient was in excited delirium.”
Because of that dubious diagnosis, Axtell was placed not in a patrol car, but on a gurney. He was strapped down and shot up with 450 milligrams of ketamine, a powerful sedative, then taken by ambulance to a hospital, then jail — even though the charges against him (which ranged from menacing to making an “offensive gesture”) were flimsy and soon dismissed.“They saw it as their right to knock people out, so they wouldn’t have to deal with them on an ambulance ride.”
tweet this
On the video, Springsteen can be heard expressing astonishment that Axtell was being sedated. Looking back on the situation now, she expresses regret that she didn’t protest more vigorously — but she also didn’t want to be accused of using her position as an elected city official to interfere. “I thought they were taking him to a squad car,” she says. “But they had normalized this so much in their minds. They saw it as their right to knock people out so they wouldn’t have to deal with them on an ambulance ride.”
Axtell has no recollection of that ride, or anything else until he woke up in the hospital seven hours later, still feeling the effects of his sedation. In a civil lawsuit he filed against the City of Lakewood and West Metro Fire, he claimed that police used excessive force in his unwarranted arrest and that the hefty dose of ketamine he received, along with other sedatives administered at the hospital without his consent, have caused ongoing physical and psychological trauma, from memory issues and urinary tract problems to insomnia and PTSD.
“It messed me up,” Axtell told state lawmakers at a hearing in 2021. “I can’t do anything right anymore.”
For years, emergency-medicine professionals have extolled ketamine as a safe, effective tool for dealing with combative or delusional patients, with reported medical complications in only a small percentage of cases. But Springsteen, who represented Axtell in his lawsuit, soon discovered that Colorado paramedics were routinely using ketamine as a “chemical restraint” in hundreds of purported excited delirium cases a year — 902 times over thirty months, or about once a day, according to a 2020 KUNC report — and that the practice had been linked to several deaths.
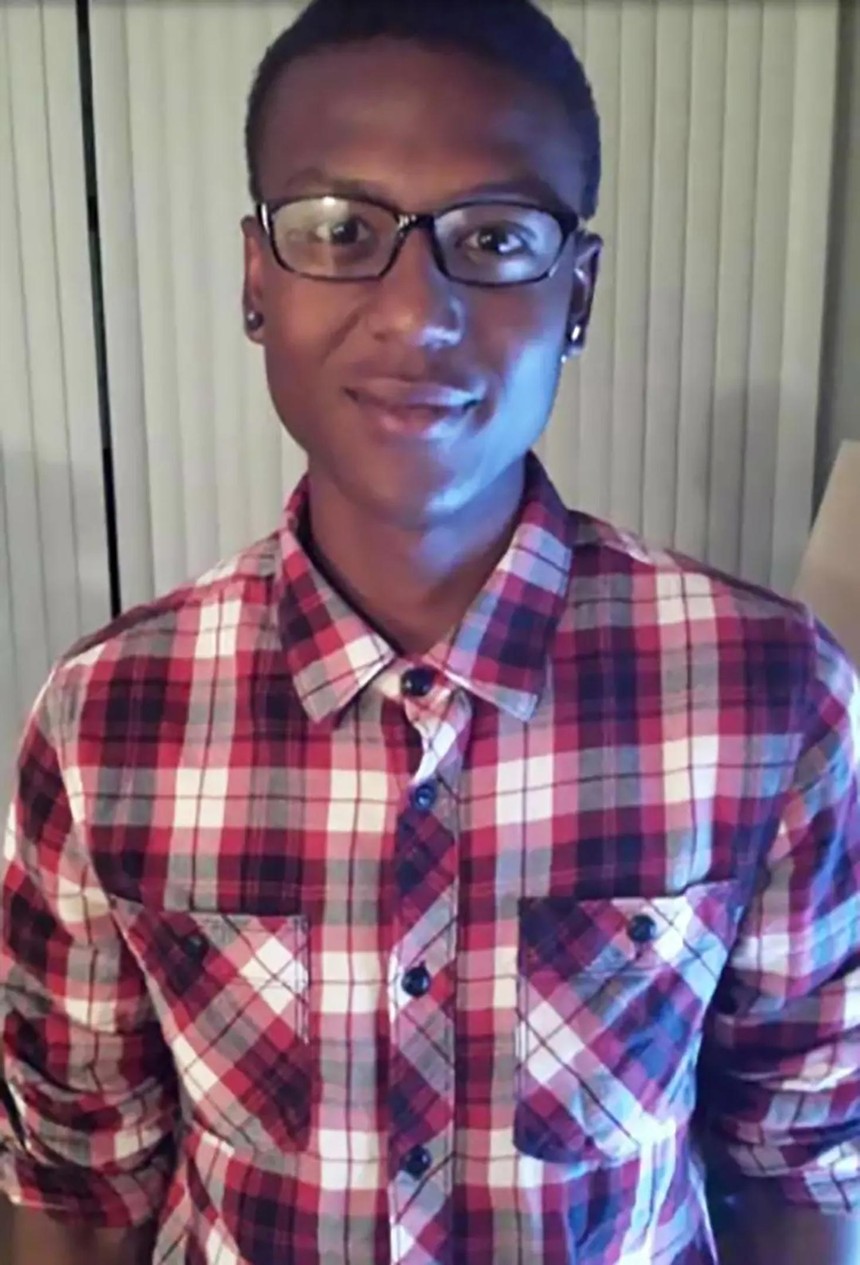
Elijah McClain, 23, was stopped by Aurora police officers on August 24, 2019.
Family of Elijah McClain
McClain’s death initially attracted little public scrutiny; the highly equivocal autopsy report from the Adams County Coroner’s Office listed cause and manner of death as undetermined. But in the wake of the 2020 George Floyd protests, the McClain case became one of several in-custody deaths drawing international attention and outrage.
The harsh spotlight eventually led to a revision of the official autopsy report, which now concludes that McClain died from “complications of ketamine administration following forcible restraint.” It also prompted an unprecedented criminal prosecution of police and paramedics who were on scene. Last spring, Peter Cichuniec, the paramedic who authorized the dose of ketamine McClain received, was sentenced to five years in prison for negligent homicide, while another paramedic, Jeremy Cooper, got probation; police officer Randy Roedema was sentenced to fourteen months in jail. Two other police officers were acquitted of all charges.
The fallout of the McClain case extended well beyond those involved in the fatal encounter. In 2021, new state legislation set tough restrictions on the use of ketamine outside of a hospital setting, prohibited police officers from influencing paramedics to sedate a suspect, and declared that the controversial “diagnosis” of excited delirium couldn’t be used to justify ketamine use. The Colorado Department of Public Health and Environment also suspended the issuing of waivers that allow local EMS agencies to administer ketamine to sedate unruly patients.
As the five-year anniversary of the McClain tragedy approaches, Colorado is widely regarded as being in the vanguard of efforts to reform the use of chemical restraint. But critics of the state’s regulatory process point out that ketamine is still being administered by paramedics across the state hundreds of times a year — albeit in smaller dosages than those given to Axtell and McClain, and for purposes other than excited delirium. But Springsteen believes the CDPHE hasn’t done enough to restore public confidence, investigate abuses by emergency medical personnel or hold medical directors accountable for what she suspects are more deaths, injuries and adverse outcomes from ketamine use than officials want to admit.
“I would really like to see somebody clean house at CDPHE,” she says. “But in order to have accountability, you first have to have acknowledgement that something went wrong.”
History of Ketamine
For a drug that has found so many different applications over the past half-century, from pain management to psychedelic exploration to the treatment of depression, ketamine has a curious origin story.It was first synthesized in 1962 by a Detroit chemist seeking to develop a safer anesthetic for surgery — one without the hallucinations, amnesia and other unpleasant effects of more established alternatives. But ketamine, a chemical analog of angel dust, also has dissociative properties. Initially used as a horse tranquilizer and as a battlefield anesthetic during the Vietnam War, it was championed by counterculture guru John C. Lilly for his psychic experiments, adopted by Hunter S. Thompson for recreational use and dubbed “Special K” by head-trippers and ravers.
How ketamine became the wonder drug for emergency medical services is a bit more complicated. As far back as the early 2000s, first responders began grappling with an increasing number of calls involving agitated and possibly psychotic individuals, fueled by some combination of street drugs — meth, cocaine, opioids — and mental illness. A few prominent agencies began looking into their pharmaceutical cornucopia for answers. Ketamine was extolled as safer and faster-acting than other sedation options, sparing police and paramedics as well as patients the risks of a physical takedown. Soon ketamine was the go-to knockout punch across most of the country.
Unfortunately, the drug was not the ideal solution it was made out to be. Some of its most vocal advocates had financial ties to the company that made tasers; a “tase and sedate” strategy was one scenario that researchers promoted as less lethal than other alternatives. And it’s doubtful that the ketamine movement would have been so widely embraced if not for the rise of a bogeyman the drug seemed designed to address: excited delirium syndrome.
Strictly speaking, EDS isn’t a diagnosis at all. The term was coined in an attempt to explain why certain people suddenly die after a struggle with law enforcement, even though there isn’t evidence of trauma or disease that would account for the death. One 2006 book on the subject by a highly respected pathologist contends that many deaths blamed on police excessive force are actually the result of EDS. In most of the cases cited, the victim was resisting restraint, high or disoriented, exhibiting extraordinary strength and, after a period of overheated and violent exertion, collapsed and died.
Such delirium was a convenient excuse for police agencies looking to elude liability for in-custody deaths. It also became a ready-made justification for paramedics to bring out the ketamine. But over time it became clear that EDS was being “diagnosed” in numerous individuals who didn’t fit the EDS criteria (like Elijah McClain, who wasn’t on drugs or mentally ill); that the EDS label was disproportionately being applied to young Black men (like McClain); that it was, in effect, junk science with an agenda.“It feels like we’ve taken a step back. We’re back to a combination of medication and restraint."
tweet this
In 2020, the American College of Emergency Physicians issued a statement cautioning against using ketamine “to chemically incapacitate someone solely for a law enforcement purpose.” Three years later, ACEP withdrew its approval of the term “excited delirium” altogether. Both actions came too late for McClain, whose case was a textbook example of misuse of the drug. The dosage he received was higher than it should have been because paramedics badly overestimated his weight. Ketamine increases the risk of stroke and irregular heartbeat and can lead to vomiting and respiratory problems; McClain had already vomited and complained of having trouble breathing after being assaulted by the police, which should have precluded an injection. And he wasn’t properly monitored after receiving the sedative, as ketamine guidelines require. Instead, he slipped into cardiac arrest twice on the way to the hospital and never regained consciousness.
His death was hardly an isolated case. A recent investigation by the Associated Press, Frontline and the Howard Center for Investigative Journalism found at least 94 deaths nationwide from 2012 through 2021 linked to the use of ketamine or other sedatives during police/paramedic calls. That’s about 10 percent of all law enforcement restraint deaths reported for those years.
As Springsteen discovered in the course of her own ketamine research, several of those deaths were in Colorado. A few of them even made the local news, though none attracted the firestorm of attention surrounding McClain’s death:
• In 2018, deputies and paramedics in Colorado Springs responded to a trespassing report and found Jerica LaCour, 29, curled in a fetal position and weeping in a parking lot. Over LaCour's protests and those of a firefighter on scene, paramedic Jason Poulson injected the mother of five with ketamine. She died minutes later; an autopsy report attributed the death to “respiratory arrest associated with acute alcohol and ketamine intoxication.”
• In 2020, Geno Fuentes, 42, complained of chest pains while incarcerated at the Trinidad Correctional Facility. A private ambulance company responded, but there were unexplained delays in transporting Fuentes, who died after unsuccessful attempts to resuscitate him. The official autopsy report states that Fuentes died of coronary thrombosis, but it also notes a high level of ketamine in his system — not an optimal treatment regimen for someone with heart problems.
• In 2020, Mark Barr of Colorado Springs called 911 out of concern for his 26-year-old son, Hunter, who had taken LSD and cough syrup. Although Hunter Barr was quickly subdued by police, in handcuffs and face-down on the ground, paramedics decided to give him ketamine before transport. He was pronounced dead at the hospital. The autopsy report listed the cause of death as “toxic effects of ketamine” and noted a “lethal” level of the drug in his blood samples.
According to CDPHE data, from 2000 to 2024 there were seventy deaths in Colorado involving ketamine. Sixteen of those fatalities were attributed to suicides or death by natural or undetermined causes, with ketamine present in the system; the other 54 are described as “unintentional drug overdoses where ketamine was present alone or in combination with other drugs” — a category that includes self-inflicted overdoses as well as those inflicted by paramedics.

In this August 24, 2019, body camera video, Elijah McClain is pinned to the ground while Aurora paramedics prepare to inject him with a sedative.
Aurora Police Department/Howard Center for Investigative Journalism
A month after McClain’s death, during a traffic stop in Manitou Springs, Steven Reycraft suffered a head laceration and was shot up with ketamine and Versed, a pre-surgery drug that’s also used by some states as part of the lethal-injection brew in executions. Reycraft’s lawsuit over the incident was dismissed.
So, too, was the lawsuit brought by Jeremiah Axtell after his ketamine experience. Springsteen says it’s difficult to overcome governmental immunity standards in chemical restraint cases, particularly when the regulators don’t seem inclined to punish syringe-happy paramedics. She was unable to find any evidence that CDPHE has disciplined anyone over the Fuentes and Barr deaths or even conducted an investigation of the circumstances; Poulson, the paramedic in the LaCour case, had his certification status placed on “probation” until late 2023, but records indicate he is currently certified.
Springsteen filed a complaint with CDPHE about the paramedics’ actions in Axtell’s case. She received a letter stating that the department had investigated the matter thoroughly, including “interviews and meetings with persons with knowledge of the event in question,” and determined there were no grounds for disciplinary sanctions. But that investigation didn’t involve talking to Springsteen, an eyewitness, or viewing her video, which contradicts the paramedic’s account of the incident.
Often, it seems, the truth about ketamine comes on a slow drip over a long time. In his original autopsy report for Elijah McClain, forensic pathologist Stephen Cina offered a grab bag of possible explanations for his death, including the possibility that “the Decedent had an undiagnosed mental illness that led to Excited Delirium.”
Cina’s amended report, released nineteen months later, makes no mention of excited delirium. It’s as if the whole syndrome that led to the rise of chemical restraint, the dragon that ketamine was supposed to slay, had never existed in the first place.
Putting Controls on Ketamine
In late 2021, a special ketamine review panel convened by CDPHE released a report that rejected the fuzzy diagnosis of Excited Delirium Syndrome, stating that “it lends itself to discriminatory practices.” The report was a little late to the party; earlier that year state lawmakers had pushed through a measure overhauling ketamine use in a pre-hospital setting, House Bill 21-1251, that expressly forbids using a diagnosis of EDS to justify chemical restraint.State Representative Leslie Herod, one of the sponsors of 21-1251, recalls that emergency medical service providers turned out in force to oppose the bill. Some of them predicted dire consequences if they no longer had the discretion to use ketamine to protect themselves as well as their patients — including the possibility that paramedics would abandon the profession rather than face lawsuits and prosecution for daring to sedate someone. As Herod sees it, none of those ruinous outcomes have occurred.
“We haven’t seen any kind of adverse effect,” Herod says. “We are seeing less instances of excessive force. I feel it is definitely working. I don’t think this is the end of a conversation about chemical restraint, but we need to let the law play out.”
Nothing in the new law flat-out prohibits paramedics from using ketamine for sedation. It does, however, tighten up the protocols they are supposed to follow with respect to dosage, monitoring, command approval and the conditions of a “justifiable medical emergency.” Most of the provisions of HB21-1251 are directed not at EMS providers, but at law enforcement. The measure essentially sets up a firewall between first responders to keep cops from trying to influence paramedics’ ketamine use and provides criminal penalties for officers who push for sedation or fail to report others who do so.
Scott Sholes, the EMS chief of the Durango Fire Protection District and vice president of the Emergency Medical Services Association of Colorado, says that one of the new law’s biggest impacts was on “how we interact with our partners in law enforcement.” That’s not necessarily a bad thing, he adds, as it compelled paramedics to re-examine their roles and responsibilities on scene.
“We clearly have one foot in public safety,” Sholes says, “but the other foot is squarely in health care, and the cornerstone of that should be compassionate patient care. We learned that we have to do better.”
Sholes says that his many of his colleagues were uncomfortable with the prospect of proper ketamine use being dictated by a bill: “We had legislators without medical backgrounds making medico-legal history, based a great deal on emotion.” But the challenges of the new law and the prosecution of the paramedics in the McClain case were also opportunities for educating, training and improving performance, he adds.
At the same time, Sholes has seen the new restrictions force providers to return to old ways of doing things, including physically restraining patients who are combative, a high-risk scenario for injury. “It feels like we’ve taken a step back,” he says. “We’re back to a combination of medication and restraint. We’re back to medications that are slower-acting and less likely to work. Ketamine was so easy to give — and it worked really, really well. In the end, I feel we lost a vital tool.”
Yet ketamine is still in the tool box, to some extent. According to reports compiled by the CDPHE, ketamine was administered by EMS agencies across the state 1,703 times during the latter half of 2022 and the first half of 2023, a nearly 15 percent increase over the previous year. The reports don’t specify why ketamine was injected in each instance, but these days ketamine is mainly used for pain management of trauma victims or to make it easier to intubate a patient, a process called rapid sequence induction.
Sholes says many paramedics will opt to use fentanyl or other drugs for pain, but modest doses of ketamine remain a popular alternative. The complication rate is said to be low, but exact figures are hard to come by, since the data field for “complications” is missing or not filled out in hundreds of the reports on ketamine use filed with the state every year. (A CDPHE spokesperson says the agency has toughened its reporting requirements in recent years to obtain more complete and timely information.)
Springsteen is troubled by the omissions and loopholes that still surround ketamine use. Although she helped draft HB21-1251, she now calls it “very faulty legislation.”
“I don’t think it solved the underlying problem,” she says, “which is that the people who are supposed to be regulating this are actually buddy-buddy with the providers. They think their job is to protect EMS from the public.”
For the past four years, Springsteen and activist Frank Sturgell have been locked in an open-records battle with the CDPHE over the release of the (now long suspended) two-page waivers that were issued to dozens of EMS agencies, authorizing them to use ketamine in cases of excited delirium. Attorneys for the state have argued that Sturgell’s requests didn’t follow proper procedure; Springsteen insists that officials have stonewalled and sought unreasonable fees to release the documents. Last week, the Colorado Court of Appeals overturned a district judge's dismissal of the case and sent it back to the lower court for further review.
Springsteen doesn’t know why the department has been so opposed to handing over the waivers. But she and Sturgell have managed to obtain a few of the documents from other sources and believe they raise questions about whether CDPHE was properly approving and overseeing ketamine use.
“The paramedics were just doing what they were told to do,” Sturgell says. “Behind them was a doctor, and they were using his license to be allowed to do this. Nothing happened to the doctors or their medical licenses, not even after they killed Elijah McClain. The people who were pushing this took no responsibility.”
A new law that went into effect last month puts the CDPHE in charge of licensing ground ambulance agencies, which had previously been overseen by county officials. The move should help in developing consistent statewide standards for ketamine use. But there is no law on the books that prevents EMS providers from seeking authorization to bring back ketamine as a means of chemical restraint. A CDPHE spokesperson says there have been no recent discussions among department leadership about issuing such waivers or any requests for them.
After four years on city council, Springsteen decided not to run for re-election last year. Too much harassment, she says, too many smears and death threats for asking uncomfortable questions. At one point, someone broke into her house while she was out of town and flooded it. She figures she can be more effective as an attorney than a politician, especially in exposing the dangers of chemical restraint.
“This started out personal,” she says. “It was so traumatic to have this happen to someone I care about. But it became a quest. It made me an activist. I think it’s horrific that the government can so boldly take someone’s civil rights away.”